CASE OF THE WEEK
2020-51 / December 21
Contributors: Connie Liao, Kiril Trpkov
A previously healthy woman in her late 30s presented with a flank pain. A 9.5 cm left renal mass was seen on imaging.
Quiz
1. What is the correct diagnosis?
a. Translocation associated renal cell carcinoma
b. Perivascular epithelioid cell neoplasm (PEComa)
c. Clear cell renal cell carcinoma
d. Eosinophilic, solid and cystic renal cell carcinoma
e. Adrenal cortical carcinoma
2. What genetic alteration may be associated with this neoplasm?
a. RET mutation
b. VHL mutation
c. FCLN mutation
d. Xp11.2 translocation
e. MMR deficiency
1. b
2. d
1. Perivascular epithelioid cell neoplasm (PEComa)
2. Xp11.2 translocation
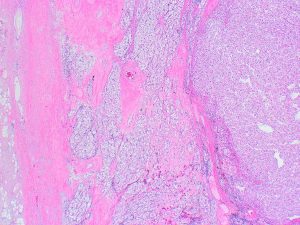
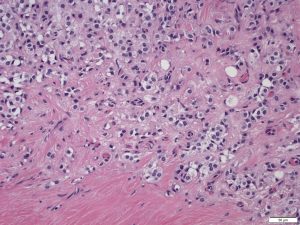
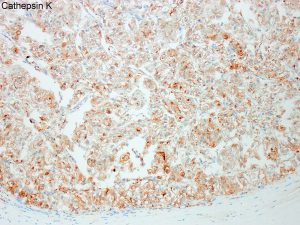
Perivascular epithelioid cell neoplasm (PEComa) is a rare mesenchymal neoplasm with melanocytic differentiation. In this particular case, PAX8 and AE1/AE3 were negative, while HMB45 and cathepsin K were positive, as illustrated. FISH revealed an abnormal TFE3 (Xp11.2) gene rearrangement.
Recent literature suggests that a subset of PEComas harbor Xp11.2 translocation (1, 2), and this is not only restricted to renal PEComas, but has been also found in PEComas of uterine and soft tissue origin. Xp11 translocation PEComas show morphologic and immunohistochemical phenotype that overlaps more with conventional PEComa than with renal cell carcinoma. Renal PEComas demonstrate mostly a nested pattern and lack overt tubules or papillae. Xp11 translocation PEComas are reactive for cathepsin K and HMB45, but not for cytokeratins or PAX8. In contrast, Xp11 translocation renal cell carcinomas with the same gene fusions are typically PAX8 positive and cathepsin K negative. They exhibit minimal to no immunoreactivity for muscle markers.
Xp11.2 translocation renal PEComas typically affect younger patients and are not associated with tuberous sclerosis complex or other hereditary disease. They have a striking female predominance and almost always demonstrate an epithelioid morphology. Although criteria for malignancy in PEComas have not been clearly established, the clinically aggressive PEComas were larger and showed marked nuclear pleomorphism, increased mitoses, necrosis, and infiltrative margins (2). Metastatic disease has also been documented (1).
1. Argani P, Illei P, Netto G, Ro J, Cho HY, Dogan S, Ladanyi M, Martignoni G, Aulmann S, Weiss SW. A Distinctive Subset of PEComas Harbor TFE3 Gene Fusions. Am J Surg Pathol 2010; 34: 1395-1406.
2. Agaram NP, Sung YS, Zhang L, Chen CL, Chen HW, Singer S, Dickson MA, Berger MF, Antonescu CR. Dichotomy of Genetic Abnormalities in PEComas With Therapeutic Implications Am J Surg Pathol. 2015;39:813-25.
Connie Liao, chiuhsiang.liao@albertahealthservices.ca
Kiril Trpkov, kiril.trpkov@albertaprecisionlabs.ca
Kidney
renal mass, PEComa